There’s something else behind the stomach – and that’s the pancreas. That’s how we learned it at school. In its first role, the pancreas is a vital digestive gland. In the unborn fetus, it is already developing on the 28th day and the Langerhans islet cells can be seen in the 8th and 9th week. Multipotent stem cells remain in the pancreas throughout their life, because they have to constantly produce replenishment, as a pancreatic cell only lives on average for about 40-50 days.
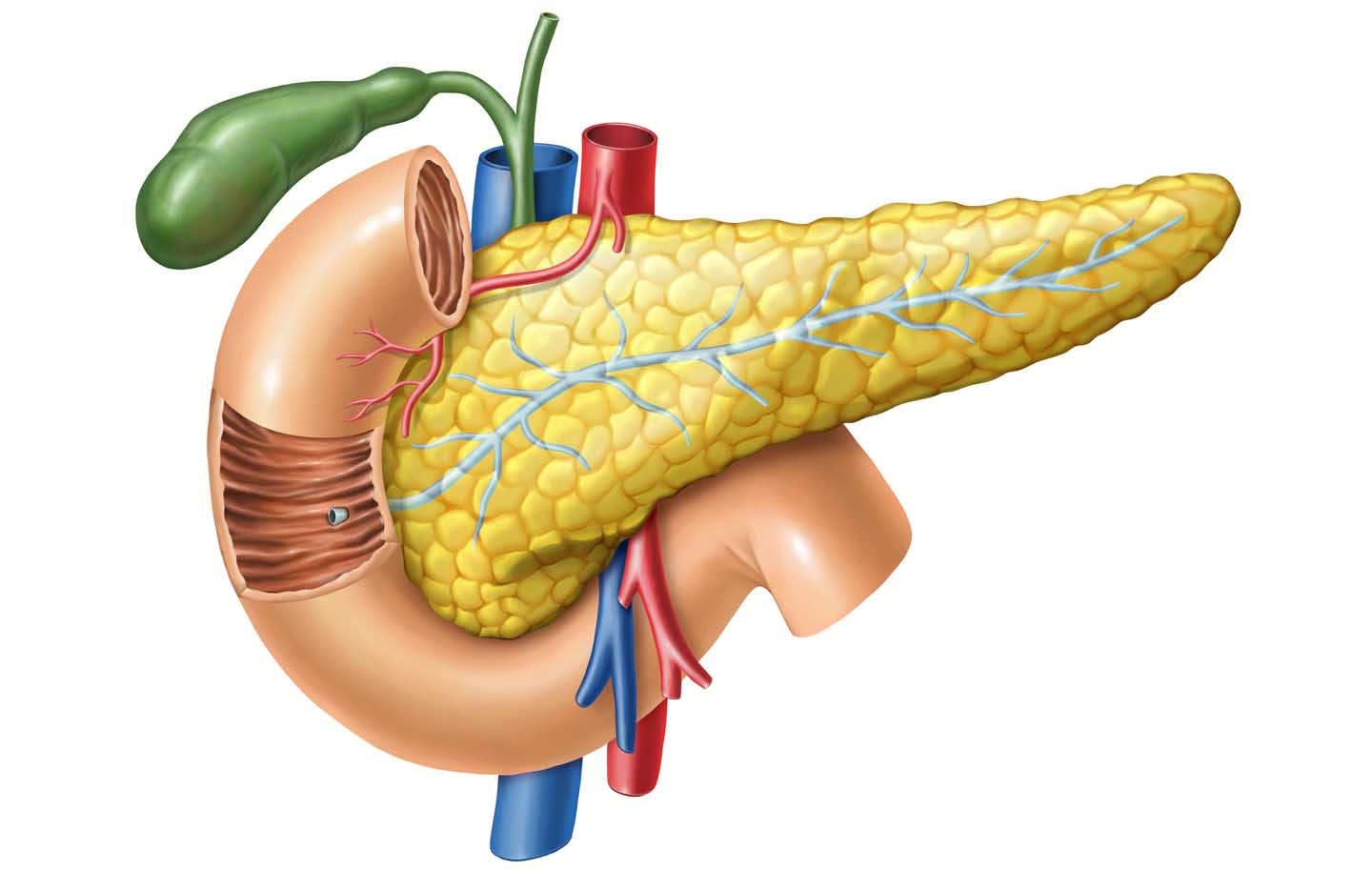
The pancreas is a relatively large gland that lies across the body behind the stomach between the spleen and liver. It is about 5-8 inch (14-20 cm) long and weighs 70-100 g. It is divided into head, body and tail. It is connected to the duodenum via an outlet duct. The duct runs the entire length of the gland. In most people, the main bile duct, the outlet from the gallbladder, unites with the outlet duct from the pancreas. They then flow together into the duodenum.
This junction can be different in some cases. In about a third of all people, both passages lead separately into the duodenum. This is an advantage, for in case that a gallstone sticks at the common duct after the union, it can lead to a backflow of digestive juice and bile in the pancreas and thus to a life-threatening inflammation of the pancreas (acute pancreatitis).
Exocrine Pancreas
The pancreas contains two parts with very different tasks: the exocrine and the endocrine part. Endocrine is called everything that secretes into the bloodstream and exocrine to the outside, in this case to the duodenum at the beginning of the colon. Note that anatomically speaking, the gastrointestinal tract is considered a tube that is a link of the body with the outside world. The pancreas is made up of several thousand lobules that are barely visible to the naked eye. These in turn are composed of several hundred glandular end pieces, the acini. The secretion of the acini is conducted into the duodenum via a duct system.
About 1.5 – 2 quarts (1.5 – 2 liters) of secretion are produced daily. The most important components are various digestive enzymes: lipases for digesting fat, amylases for digesting carbohydrates and various proteases for digesting protein. Most digestive enzymes, however, are formed in a preliminary stage, which are only converted into the active form inside the duodenum. This prevents the pancreas from digesting itself.
About 95% of the digestive juice consists of water. It is quite important that this juice is rather liquid and that the pH is around 8. In about one in 2000 newborns, the pancreatic secretion is very viscous due to a genetic defect and the pH is almost neutral. As a result, the environment in the duodenum is too acidic and fat digestion cannot function properly. It comes to fatty stools. In the pancreas itself, the ducts are blocked by the viscous secretion. The genetic defect affects various organs of the body. Even in the lungs occurs some blocking and scarring. The clinical picture is called cystic fibrosis.
Pancreatic carcinoma is the third most common tumor of the digestive tract after colon and stomach carcinoma. Smoking, frequent coffee consumption, type I diabetes and chronic pancreatitis can all increase the risk. The prognosis for pancreatic cancer is usually very poor, since rarely an early diagnosis is made, and at this point large parts of the pancreas or all of it have to be removed, often including part of the duodenum. 70 – 80% of cancer cases originate in the exocrine pancreas.
Endocrine Pancreas
The pancreas contains clusters of cells that form small islands within the tissue. They are named after their discoverer, the German physician Paul Langerhans – islets of Langerhans. These are collections of cells with a diameter of 0.1 to 0.4 mm. An adult has about a million of them. This corresponds to 2% of the pancreatic weight. They belong to the endocrine system and release their substances directly into the bloodstream.
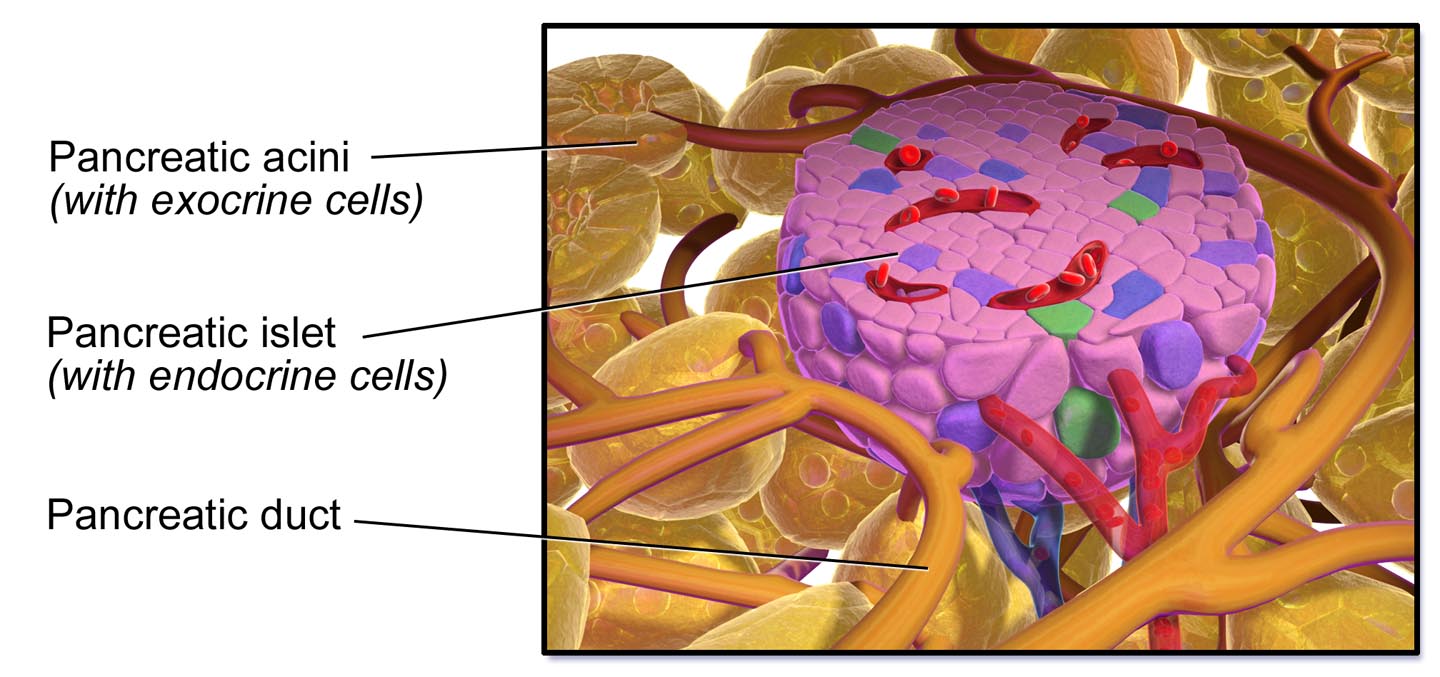
The main function of these islands is to regulate blood sugar levels. Approximately 70% of islet cells produce insulin. These cells are called Beta cells. 20% are Alpha cells and form glucagon, the counter hormone to insulin. The Delta cells make up 5% and form somatostatin, which even in small amounts prevents the release of glucagon. Another 5% make up the PP cells. PP, the pancreatic polypeptide, consisting of proteins, increases the mobility of the small intestine. This is very important for digestion so that the chyme is well mixed and comes into close contact with the colon wall. This way the nutrients can be better absorbed.
Conductive Pathways
The pancreas is permeated by nerve tracts, lymphatic vessels, lymph nodes, arteries and veins. Blood is supplied through several arteries. It is supplied by a double vascular ring. The smallest veins, the capillaries, have tiny “windows” through which the endocrine cells are in direct contact with the blood. This way the cells “feel” the blood sugar level, so to speak, and the hormones can be released directly into the bloodstream.
Glucose Regulation
Regulating blood sugar levels is very important. The carbohydrates are released into the bloodstream in the form of glucose. The concentration in healthy adults is around 80-100 mg per 100 ml of blood. The two main hormones involved in regulation come from the pancreas: insulin and glucagon. They are opponents. Insulin lowers sugar levels and glucagon increases them. After a meal, the glucose is absorbed into the blood. The blood sugar level rises. In healthy people, this causes insulin to be released into the blood, which has the function of lowering sugar levels back to normal. The insulin opens the way for glucose to enter the body’s cells. There glucose is converted into energy, where it is supposed to be used for movement, heat production and other purposes. However, insulin also causes the excess glucose to be channeled into the liver or muscles. There glucose is converted into glycogen to be stored for the use of intervals between meals.
If the sugar level falls below normal (work, fasting), glucagon stimulates the liver to release glycogen, converting it into glucose which is released back into the bloodstream. The sugar level rises again. Renewed food intake will start the whole process all over again. Continuous food intake, such as constant snacking, overstrains this control loop, which sooner or later fails, leading to type II diabetes mellitus. Obesity also promotes the development of diabetes. This type used to be referred to as adult-onset diabetes. However, because patients with diabetes are getting younger and younger due to an unreasonable lifestyle, this term has been abandoned.

Sometimes oral anti-diabetic drugs are used to increase the release of insulin from the Beta cells and can be used to treat type II diabetes. If the lifestyle is not corrected, their effectiveness is normally weaning with time.
Type I diabetes is an autoimmune disease with targeted destruction of the Beta cells that produce insulin. This diabetes can only be treated with insulin injections. Beta cells can also be damaged by viral infections. Research suggests that certain components of cow’s milk, if administered to infants whose intestines are still permeable, can trigger an autoimmune response that damages the Beta cells. So it really makes sense to breastfeed the newborn for as long as possible.
Even if the Delta cells are damaged, for example by a tumor, the blood sugar rises. Tumors affecting PP cells cause severe diarrhea.
We see that our pancreas is a very important organ for our digestion and the whole metabolism. We do well to take good care of our pancreas. We shouldn’t overwork our pancreas by constantly snacking or eating too many meals a day. A healthy adult will do well on three meals a day. He doesn’t need any snacks. Between meals he should consume only liquids, ideally water. In his wise creative power God has implanted a very interesting organ in our body. We can only be amazed how nicely and wonderfully our entire metabolism depends on small things that are interdependent like the many wheels of a clockwork.

Stay Always Up to Date
Sign up to our newsletter and stay always informed with news and tips around your health.

Esther Neumann studied Nutrition at the University of Vienna. Since then she served as an author for the health magazine “Leben und Gesundheit” and conducted health lectures in various locations of Austria.
My, my. I had no idea how important my pancreas is and how it functions.
Thank you for this valuable article. God bless.